
The seeds of a consumer-driven health care revolution, one that could turn the U.S. health care system on its head, were sown in early March. This potential disruption comes from an unlikely source: two proposed rules from the Department of Health and Human Services that could have consumers and America’s biggest tech firms joining forces.
The rules, from the Office of the National Coordinator for Health IT (ONC) and the Centers for Medicare & Medicaid Services (CMS) are both focused on allowing consumers free and easy access to their health data and letting them opt to share that data with big tech or whomever else they chose.
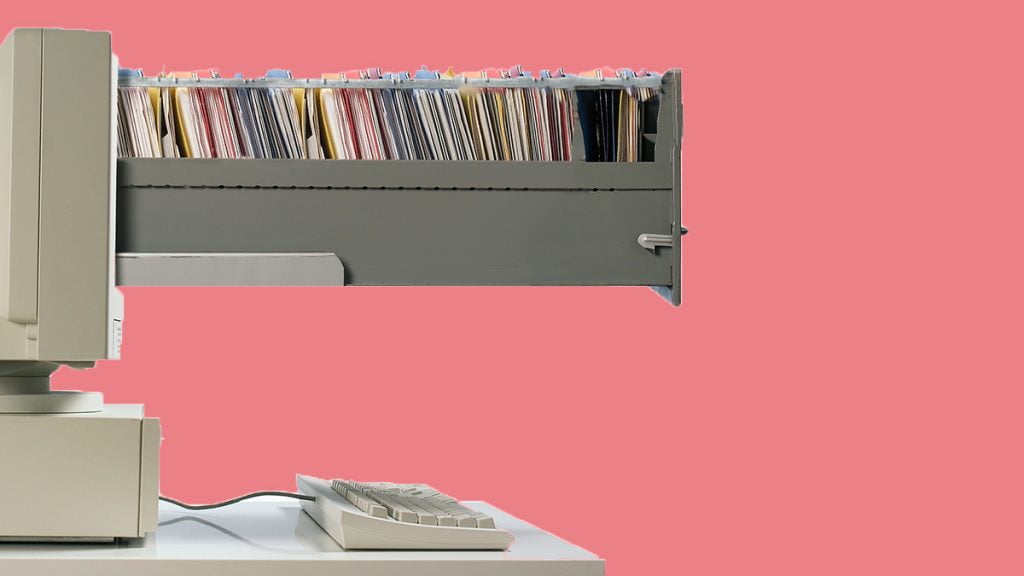
The ONC rule would require that health care providers and vendors of electronic health record (EHR) vendors make patients’ health data easily and cheaply available to them electronically. This implements provisions of the 2016 21st Century Cures Act that requires providers and vendors to adopt so-called open application program interfaces. APIs allow different programs to talk to each other. Open APIs will make it easy for consumers — acting through authorized third parties — to gain direct access to their EHRs and their personal clinical data. Think of APIs as tunnels into the clinical data warehouses that have been created by EHRs. Think of third parties as new and existing IT powerhouses — including the likes of Apple, Amazon, and Google — that have been authorized by patients to act as data stewards on their behalf.
The CMS rule aims to liberate patients’ data from another critical source: insurers. CMS is proposing to use its regulatory authority over public and private organizations that cover publicly insured individuals (e.g., Medicare Advantage plans, Medicaid Managed Care, and CHIP plans, and private plans operating in federally operated ACA marketplaces) to require that their customers’ data be easily available to them in electronic form. Insurers would have to share data not only with patients and their authorized third parties but also with other insurers if requested by patients. And once again, the technical key would be the adoption of open APIs that make it easy for patients’ designated third parties to tunnel into electronic repositories and extract health care information.
So what’s the big deal? How can all this technical mumbo jumbo revolutionize health care? Because it has the potential to open up the health care marketplace to consumer-driven competition in ways never seen before in the history of medicine in the United States or anywhere. Although the Trump administration has to weigh whatever comments on the proposed rules that interested parties submit, it has signaled support for data transparency in the past, which suggests that it won’t significantly revise them.
One reason that health care markets are so flawed and inefficient is that consumers and patients lack the knowledge to make good choices. In particular, they lack data about their own health and about the health and economic consequences of their decisions. The EHR and these new federal rules could change that fundamentally by giving patients unprecedented access to the information they need to be wise consumers of health care.
Even with data liberation, however, there is a substantial gap between theory and practice in creating functional consumer-driven health care markets. One problem is that data, by themselves, are insufficient. Many consumers are ill-equipped to make sense of the reams of detailed information that populate their EHRs and their claims repositories. They need help organizing those data and interpreting them in light of their own histories, the scientific literature, and the health care resources available to them in their own communities.
The solution: Consumers could rely on IT companies to collect, manage, and refine the data on their behalf. Thus, the reference in the rules to “authorized third parties.” The IT industry is furiously hiring clinicians to help it understand the technical and scientific aspects of health care. Their apparent goal is to assemble patients’ clinical data, the best science, and the many other data resources available to savvy IT companies, and then to mix in artificial intelligence, machine learning, and their skill in making consumer-friendly software. The hoped-for result is usable, timely, patient-empowering decision-support tools that are game-changing for health care and health care markets. Elsewhere, we have suggested that this process could lead to what we call “digital health advisers”: Alexa and Siri equivalents for health care consumers.
As a leading market indicator consider that Apple already has agreements with over 200 health care providers — both large systems and small practices — to download patients’ data (with their permission) to Apple devices using open APIs and new Apple software. It would be surprising if the secretive Apple were not already working on ways to make that data understandable and useful to consumers.
This scenario remains speculative. Other obstacles to a consumer-driven health care revolution remain. Threats to patient privacy and security abound when third parties are authorized to access patients’ data. And to the extent that those IT agents start to produce clinical advice for consumers, regulators will likely step in to require assurances of safety and efficacy. If new tools lead patients to make health care decisions that their clinicians view as unwise or possibly dangerous, a backlash could undermine their spread.
Nevertheless, with the publication of these rules, and likely further public and private actions to come, doors are opening to a health care system that may look dramatically different from the status quo. Digitizing health care data was always expected to have dramatic and unpredictable effects. True patient empowerment may be one.
[“source=hbr.org”]




