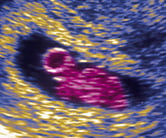

“Abnormal cells not a sure sign of baby defects,” reports The Telegraph following the publication of a study on the development of healthy embryos.
Embryos containing cells with an abnormal number of chromosomes can still develop into healthy babies, according to researchers from the University of Cambridge.
Embryo cells with too many or too few chromosomes can give rise to a number of health conditions in a newborn, such as Down’s syndrome.
Pregnant women – particularly older mothers, whose offspring are at an increased risk of developing such conditions – are offered tests to predict the likelihood of genetic abnormalities.
Between weeks 11 and 14 of pregnancy, mothers may be offeredchorionic villus sampling (CVS), a test that involves removing and analysing cells from the placenta.
If the CVS shows an abnormality, a further test called anamniocentesis is recommended during weeks 15 to 20, and involves analysing cells shed by the foetus into the surrounding amniotic fluid.
However, research using mice found embryos with 50% of defective cells could develop healthily in the womb and result in healthy mice pups.
In this scenario, the defective cells tended to self-destruct, leaving the healthy cells to continue to develop normally as the embryo continued to grow.
However, the lab study found embryos containing more defective cells than normal ones were less likely to develop healthily in the womb. The researchers saw clear implications for the assessment of embryo viability in human fertility clinics.
The study raises debate about the accuracy of screening embryos with chromosome abnormalities in pregnancy. But more research is needed before it could have a bearing on current fertility practices.
Follow-up studies in people are needed to ensure the same thing happening in mice happens in people, which isn’t guaranteed.
Contents
Where did the story come from?
The study was carried out by researchers from the University of Cambridge, the University of Leuven, and the Wellcome Trust Sanger Institute.
It was funded by the Wellcome Trust, Research Foundation Flanders and KU Leuven SymBioSys, a group of computer scientists and molecular biologists.
The study was published in the peer-reviewed journal, Nature Communications and is free to read online.
Generally, the Mail Online reported the story accurately, but focused on the personal story of Professor Magdalena Zernicka-Goetz, the lead researcher. Professor Zernicka-Goetz gave birth at 44 years old “despite a test that showed there was a high chance her child might develop Down’s syndrome”.
Mixing science and storytelling is a powerful journalistic tool, but can make it less obvious to casual readers that the main research underlying it was in mice, not people.
What kind of research was this?
This laboratory-based mouse study investigated what happens to cells with abnormal numbers of chromosomes during the early stages of embryo development.
Most cells have an even 23 pairs of chromosomes, called euploid. But sometimes there is one more or one less, creating odd numbers – called aneuploid. For example, an extra chromosome 21, an example of an aneuploid cell, gives rise to Down’s syndrome.
The researchers investigated the time shortly after a sperm fertilises an egg, when the two sex cells multiply, fold and specialise as part of a small ball of cells.
This keeps growing and dividing while travelling down a fallopian tube to implant in the womb as an early embryo – this implantation happens around nine days after fertilisation.
In previous experiments, researchers observed that early embryos contained cells that were a mix of those with 23 pairs of chromosomes (euploid) and those with odd numbers (aneuploid).
They knew that in some circumstances this mix could produce a healthy embryo, but in other scenarios it died before implantation in the womb, but they didn’t know why.
The researchers set out to uncover what was happening to the euploid and aneuploid cells early in development, and how this was related to embryo viability and key developmental stages later on, such as implantation of the embryo in the womb.
Mice are very useful when studying embryo development as they have many of the same key stages humans have, albeit on a significantly shortened timescale. You can also manipulate mouse cells in a way you can’t in people.
Ultimately, however, experiments in people are the key to moving this type of research forward.
What did the research involve?
The researchers used different genetic, molecular and cell biological experiments to track the locations of euploid and aneuploid cells in mice embryo development.
For example, in one set of experiments they artificially created early embryos – small balls of cells – containing different proportions of cells with normal (euploid) and abnormal (aneuploid) chromosome counts to measure the success rate of implantation each time.
Some contained all aneuploid cells, others were 50% aneuploid and 50% euploid, and a final set had 75% aneuploid cells and 25% euploid.
A second experiment tracked the cells in real time to see which ones grew and divided, and which ones died away, at different stages of embryo development.
What were the basic results?
Early embryos containing only cells with unusual numbers of chromosomes – aneuploid – died during development before implanting in the womb. But embryos with a mix of aneuploid and euploid cells were able to develop further and implant in the womb successfully.
Live embryo imaging and cell tracking through development and implantation showed success depended on whether the aneuploid cells were part of the placenta, supporting the embryo, or part of the embryo itself.
Aneuploid cells in the embryo itself progressively self-destructed using a cell suicide process called apoptosis. By contrast, aneuploid cells from the placenta kept dividing and growing, showing many defects along the way.
Because the embryo cells with abnormal chromosomes tended to self-destruct over time, there were progressively less of them as the embryo got bigger and bigger.
Using a straight split of 50% aneuploid and 50% euploid cells, the team showed implantation could be achieved in all of these embryos.
But this dropped to 44% success when the ratio was 75% aneuploid to 25% euploid, suggesting success depended on the ratio of “normal” and “abnormal” cells at the start.
How did the researchers interpret the results?
The team concluded that embryos with a mix of aneuploid and euploid cells “have full developmental potential, provided they contain sufficient euploid cells, a finding of significance for the assessment of embryo vitality in the clinic”.
Conclusion
This mouse study helps to advance scientific understanding of how some embryos containing a mix of euploid and aneuploid cells develop normally and others do not.
This looks to be related to the proportion of euploid and aneuploid cells early on in the cells’ development, and their specific location.
However, though the researchers saw clear implications for the assessment of embryo vitality in human fertility clinics, this research is at too early a stage to be able to accurately predict outcomes for human foetal development.
Follow-up studies in people are needed to test whether this mice observation happens the same way – which isn’t guaranteed.
The research largely measured successful implantation in mice, but also tested whether this would tell us something about successful live birth rates and subsequent development.
These experiments suggested healthy implantation was a good way of predicting healthy development at later stages, at least in mice – a strength of this study.
[Source:- NHS]




